Hollywood Medical Myths Part 1: Shocking Someone Who Has “Flat-Lined” Can Get Their Heart Going Again
Myth: Shocking someone who has flat-lined can get their heart started again.
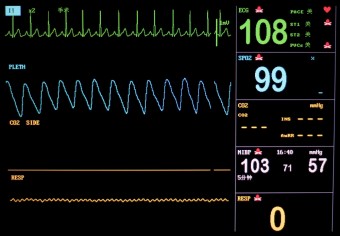 It never fails. You’re watching television and someone is circling the drain, in the toilet that is their life. The noise from the heart monitor affirms they’re still alive, with its consistent, rhythmic beeps. All of the sudden, alarms start going off. On the monitor- the dreaded “flat-line”.
It never fails. You’re watching television and someone is circling the drain, in the toilet that is their life. The noise from the heart monitor affirms they’re still alive, with its consistent, rhythmic beeps. All of the sudden, alarms start going off. On the monitor- the dreaded “flat-line”.
Doctors begin rushing in. One of them always seems to yell, “Hand me the paddles; we’re losing him!” The machine is charged, and miraculously the heart is shocked back to life, saving the day! (But only after a suitably dramatic number of zaps and someone inevitably shouting “LIVE DAMN YOU!”)
The problem is that, in real life, you’ll be accomplishing nothing by shocking a “flat-line”. Unless you like your meat well done that is.
Medically, a “flat-line” is known as asystole, meaning no (heart) contraction. It might seem common sense that if there is no contraction you might want to contract it with a shock. The truth about why this will never “restart” the heart lies in how the heart creates its life giving beat. In the end, it all comes down to electrolytes.
The heart typically receives approximately 60-100 “shocks” per minute, usually from specialized pacemaker cells in the right upper portion of the heart, known as the Sinoartrial node (SA node). These specialized cells will naturally create an electrical differential between the inside of the cell and the outside. Once that differential is at just the right amount, it will send a “shock” down, and throughout, the heart muscle causing it to contract. Once this electrical signal is produced, it will generally go completely throughout the heart through the cardiac conduction system.
You might be thinking right now, if the heart creates a shock to get a contraction, why won’t shocking it externally get the job done? Well, the devil is in the details.
The SA node creates an electrical differential using electrolytes like potassium, sodium and calcium. I won’t be going into a college level physiology lecture, as this article would be way too long and I imagine most of you aren’t interested in reading such an essay. However, for the purposes of understanding why shocking asystole doesn’t work, I will very briefly summarize what’s going on “under the hood” here.
These electrolytes all have specific electrical charges that pass through your cell walls using channels named after the electrolyte- sodium channels, calcium channels etc. Potassium generally lies inside of your cell before it contracts; sodium and calcium generally reside outside the cell. When you have a blood pressure (if you didn’t you would quickly be dead), sodium is naturally forced inside your cell. This also causes potassium to be forced out of your cell creating an electrical potential. Once that potential gets high enough, it opens up calcium channels which are voltage regulated. When the calcium channels are opened up, sodium and calcium rush inside the cell creating just the right amount of charge. Once that charge is reached, the heart sends out its shock, known as depolarization.
So where does that impulse go once the SA node creates it?
When the SA node sends out its life sustaining impulse, it immediately shocks the atria. The pulse then gets “held up” in another set of cells called the Atrioventricular node, or AV node for short. This allows for the bottom part of the heart to receive the blood from the top part. The AV node then transmits the impulse down to the bundle of His (no, not the bundle of hers, sorry ladies) and then to two pathways called the right and left bundle branches. It then gets transmitted to the rest of the Ventricles through what are called Purkinje fibers. All together this “shock” causes the atria to contract, then the ventricles. The wonder of a pulse!!
This electrical conduction is what doctors are looking at when they are staring at the heart monitor. Generally speaking, this impulse creates a squeeze that actually creates your pulse. There are times however, that this isn’t the case. A person could have a normal looking electrical conduction on the monitor and still have no pulse. The phenomenon is known as Pulse-less Electrical Activity (PEA). This is one of the reasons why doctors still need to check pulses, and blood pressures, even if the person is hooked up to a heart monitor.
When someone is in cardiac arrest and has no pulse, depending on how the electrical conduction system is working, they might need to be shocked. There are numerous electrical rhythms that can present themselves in cardiac arrest. I will touch on the most common, and why shocking works.
The most common heart rhythm just after someone goes into cardiac arrest is known as Ventricular fibrillation. When the SA node fails to create a beat, countless other cells within the heart attempt to create the beat instead. The result is numerous areas of the heart that “shock” it all at the same time, from different directions. Instead of a steady contracting beat, what you get is a heart that looks like it’s having a seizure.
The effect is a heart that doesn’t pump blood through it. The only way to get all of these different areas of the heart (foci) to work in unison again is to shock it with more electricity than the cells themselves are creating.
When you shock these cells with this large amount of electricity, it forces all of the electrolytes out of the cells at the same time. The hope, and it’s really just a hope, is that the heart’s normal operation of electrolytes passing across the cell membranes in an organized fashion will take over again.
Here is the devil in the shocking details.
When someone is in asystole (flat-lined), there is no electrical differential that the monitor can pick up. Essentially, there are no specific electrolytes inside the cell, compared to outside the cell, with different electrical potentials to create an impulse. If you attempted to shock this, you wouldn’t be doing anything. There are no electrolytes to force out of the cells that are any different than the ones that are already outside the cells. All you would get is more flat-line.
In fact, after every shock ever given to someone in cardiac arrest, the rhythm created for a few seconds is asystole, with the heart rhythm temporarily stopped. It takes a few seconds for the normal pathways to get going again. If you had asystole before you shocked it, all you would do is burn the heart with the heat created from the shock. As every steak lover knows, don’t burn the meat! Medium-well please… unless you’re in Texas, then from my experience it’s “rare” only and ordering anything different will see the chef come out from the kitchen and slap you in the face. (Note: The red juice in such rare red meat is not actually blood)
In the end, it’s a Hollywood myth that you would treat asystole (flat-line) with a shock. You must first have some sort of electrical impulse to work with. Science 1, Hollywood 0.
If you liked this article, you might also enjoy our new popular podcast, The BrainFood Show (iTunes, Spotify, Google Play Music, Feed), as well as:
- Does Sex Before an Athletic Event Really Hinder Performance?
- Does Reading in Dim Light Really Damage Your Vision?
- Is a Dog’s Mouth Really Cleaner than a Human’s Mouth?
- Top 5 Life-Saving First Aid Tricks Everyone Should Know, According to a Paramedic
- Alcohol Does Not Kill Brain Cells
Bonus Facts:
- According to the American Heart Association, approximately 383,000 cardiac arrests happen outside of the hospital every year inside the United States. 88% of them occur at home. Learn CPR people!
- Mechanically, the only way to get blood flowing inside the body when someone is in cardiac arrest is CPR. Early CPR, combined with early defibrillation (shocking), is the best way to save a person’s life who has gone in to cardiac arrest.
- Like most of the body, the heart does not receive blood flow when it contracts, called systole. The heart receives its blood flow when it relaxes, called diastole. This is why when someone has an extremely fast heart rate, like say 180, the person could feel light headed due to the fact that their blood pressure will be low. This is because there isn’t enough time between contractions for the heart to receive enough oxygenated blood.
- The pulmonary arteries are the only arteries in the body that carry de-oxygenated blood. Conversely, the pulmonary veins are the only veins in the body that carry oxygenated blood.
- The highest heart rate I have personally seen was 302. Yes, the person was conscious, and yes I did keep the “rhythm strip” to prove it! And yes, the person did eventually receive a pacemaker after several surgical attempts to “rewire” their heart. No I have not just broken any HIPPA laws by telling you that!
- The slowest heart rate I have seen, in a conscious person, was 28. And yes, they also received a pacemaker. (Editor’s Note: I once personally got down to 14 while conscious, though couldn’t see, my hearing was almost gone, and my body felt like I’d just been traipsing through the Mojave Desert for a few days without water. But still conscious! No pacemaker yet! Also, the makers of the tilt table really need to make it so they go back to horizontal faster. ;-))
| Share the Knowledge! |
|





Hello Scott, i have recently suffered from a Hemiplegic attack and my Neurologist has suggested that i consider going on a course of Calcium Blockers. Is this anything you know about? it seems that it is linked and i didn’t have an understanding of why calcium blockers would make any difference, but your article has flipped on a few lights for me.
Funny !! The same article was run by Gizmodo too today ?
@Tom Alex: Their editors watch TIFO pretty closely and have full permission to re-publish anything as they please, with of course proper credit and links and all that good stuff which they do.
http://circ.ahajournals.org/content/122/18_suppl_3/S729/F1.large.jpg
You are looking at the ACLS Algorithm for Adult Cardiac Arrest.
Why didn’t you mention ACLS, AHA, or the Circulation Journal in the article which goes over the reasons behind the algorithm, and why shocks are in the steps to treat asystole? (http://circ.ahajournals.org/content/122/18_suppl_3/S729.full)
As a paramedic background, shouldn’t this have crossed your mind when writing the piece? Now it’s spread to Gizmodo and thus, misinformed medical knowledge to the mass. People will smugly joke about medical scenes when they shock patients when asystole, which should be done as is written in the algorithm.
As per the algorithm, a shockable rhythm in cardiac arrest is ventricular fibrillation or pulseless ventricular tachycardia. If a patient has asystole (flat line)or pulseless electrical activity, you do CPR. After 5 cycles or 2 minutes, you will reassess the patient. If the rhythm is now shockable (see previous), you can defibrillate, however if it is still asystole, you continue CPR.
As a physician and ACLS instructor, this is one of the common misconceptions in movies that also irritate me.
I’ve known this for a while. (CPR instructor told us) What’s bothered me (and why I read this article) is what do they actually do to restart someones’ heart after flat lineing?
@Tim: I’ll ask Scott to come chime in because he’s obviously the expert in this and I’m only very vaguely remember what he’s told me before on this issue, but I believe they can do things like introduce various chemicals into the body to help try to get the conditions just right. But I could be remembering the details wrong. Again, I’ll email Scott and have him come here and chime in on this.
I’m very sorry. I am wrong. I misread the algorithm – Scott is correct.
You do not shock if asystole.
Sorry, I was the one spreading bad medical information.
@Seungjin Kim: You have misread the AHA guidelines. Follow the links you sent me. The first step says “shockable rhythm” no= asystole and PEA, yes= VF/VT. So it is wrong to say that the AHA has recommended shocking someone in asystole. As you have stated, my paramedic background has me extremely familiar with these guidelines as we are required to have them memorized.
@ Tim; This is a very complex question to answer. The medications we give to people in this situation do not, in and of themselves, actually put someone back in to a “shockable” rhythm. Depending on numerous factors we give certain medications in the hopes of reversing the cause of the arrest and hope this helps in putting someones natural electrolyte environment back to a more normal state. They are known as the H’s and T’s. Hyper/hypokalcemia (high and low potassium) hypothermia, hypoxia, trauma, toxins, etc. etc. When someone is in asystole the standard of care right now is to give epinephrine or vasopressin combined with great CPR compressions. Epinephrine is just a hormone that acts on several different types of cells (alpha and beta), but doesn’t necessarily “re-start” someones sodium/potassium pump in their SA node. Vasopressin is just a drug that acts on alpha cells resulting in the constricting of your arteries. The prevailing thought in the medical world is that this will help CPR compressions give more blood flow to the areas needed and thus help in the exchange of electrolytes during compressions and put them back in to a more homeostatic state. (and also helping in blood pressure should you get a shockable rhythm back) Given the fact that the current survival rates for cardiac arrest in asystole are somewhere in the neighborhood of 4% (depending on the study you read) you can see that these approaches, while the only options we have right now for medicines, don’t do as good of a job as we would like. I hope that helps.
@ tim, I meant hyper/hypokalemia not kalcemia. Mistype
Please, could you clarify if I got it correct:
– Flat-line implies no-pulse and implies death most of the times.
– No-pulse does not necessarily implies flat-line. Other questions: what happens with the cardiac activity when someone is struck by a lightning? Can he/she be revived by a shock (ironic)?
I know this is almost a year late, but I’ll respond to Héctor’s comment …
(1) Yes. Asystole (flat-line) implies no pulse (unless there’s an equipment malfunction / user error / etc). And yes, most folks who are in Asystole “stay dead.” But not all.
(2) All four rhythms of cardiac arrest (Ventricular Tachycardia, Ventricular Fibrillation, Asystole, Pulseless Electrical Activity) imply no pulse. Essentially, cardiac arrest = no pulse. But different things may show up on the monitor, and depending on which rhythm it is, that changes the treatment given by the medical professional.
If someone was struck by lightning and is put into cardiac arrest, I think it’s most likely that they’d be in Ventricular Fibrillation first. If so, then yes, they could be revived by a shock if it is given in time. V-fib will eventually turn into Asystole if nothing is done.
A medic / doctor / etc. shocking a heart is basically like a computer tech performing a reboot. The idea is to shut everything off (the chaotic electrical activity) and get it to restart properly.
If there’s an organized rhythm with no pulse (PEA), then it shouldn’t be shocked because the rhythm is fine – there’s another problem that must be fixed. If there’s no electrical activity at all (Asystole), there’s no point in shocking because there’s nothing to reset.
It’s HIPAA, not HIPPA. But great article!